iPSCs and other stem cells
Allele Receives NIH Award to Fund the Development of Large-Scale Stem Cell Production
SAN DIEGO–(BUSINESS WIRE)–
The NIH’s National Heart, Lung, and Blood Institute has awarded Allele Biotechnology and Pharmaceuticals (“Allele”) a Phase 1 SBIR grant to develop a novel manufacturing system to produce stem cell-derived human tissue and cells for clinical therapy. By increasing the scale of production and reducing the cost of manufacturing, Allele is confident that this system will overcome a considerable roadblock for clinical applications of stem cells, which is to produce a sufficient amount of therapeutic material at a manageable cost.
At the core of translating this potentially game-changing technology into medically-beneficial applications is the use of induced pluripotent stem cells (iPSCs), which hold unprecedented promise of providing any type of immune-matched cells of unlimited quantity. Allele has already developed a patented method of reprogramming somatic cells into iPSCs, secured industrial licensees using this technology, and initiated cGMP procedures for clinical applications.
Further moving iPSCs into commercially viable clinical cell therapies still requires overcoming one major barrier: the prohibitive cost of manufacturing iPSC-derived cells, mostly due to the need of expensive clinical-grade growth factors and cytokines. For example, the estimated cost of the growth factors and cytokines needed to produce a typical transfusion of platelets is $87,252.
Ultimately, Allele’s goal is to create clinical-grade iPSCs and control their differentiation into specific cell types at a scale large enough to satisfy the clinical demand. “We have been diligently working on removing the use of protein factors through our own proprietary protocols to generate many clinically-relevant cell types, including beta cells, mesenchymal stem cells, neural progenitor cells, oligodendrocytes, liver, and heart cells,” said Dr. Jiwu Wang, Allele’s CEO and the Principle Investigator of the new NIH grant. “By developing a recombinant protein-independent, real-time adjusted culture system under this project, we are confident that—as many groundbreaking technologies such as genome sequencing have done—the manufacturing process will mature and the costs will come down to eventually benefit everybody.”
Allele’s plan gained trust from the NIH scientific review panel, which gave it a near-perfect score. With this funding, Allele’s researchers will move even faster towards the goal of bringing iPSC products to clinical applications. Successful efforts will also likely provide a vehicle for genome-editing technologies such as CRISPR to be delivered into patients.
View source version on businesswire.com.
Stem Cell Therapies: What’s Approved, What Isn’t, and Why Not?
With acceptance of stem cell therapies growing, so have controversies surrounding regulations.
Desperate to heal sports injuries, top professional athletes have been known to pay tens of thousands of dollars for experimental stem cell treatments that many used to find controversial. But now, stem cell therapies have become more mainstream and are no longer limited to professional athletes. Stem cell clinics offer both medical and non-medical treatments with claims of improving aesthetics and quality of life.
One recent study found over 400 websites – with the largest portion in the United States – advertising stem cell-based therapies (1); another found over 570 U.S. clinics offering stem cell interventions (2), giving more evidence that the market for stem cell therapies in the U.S. is growing at an accelerated rate. Yet these therapies are too often based on unfounded claims and lack proper clinical trials or authorized regulation. Despite what some clinics claim, very few stem cell treatments are currently available that are actually approved by the Food and Drug Administration (FDA). Hematopoietic stem cells harvested from bone marrow are routinely used in transplant procedures to treat patients with cancer or other blood or immune system disorders. Banking of umbilical cord blood is FDA-regulated and its use is approved for certain indications. Otherwise, consumers should be wary of claims by stem cell clinics implying FDA-approval.
So why aren’t more FDA-approved stem cell therapies available?
The FDA has strict regulations on using stem cell products in humans. In most cases, stem cell-based products are categorized the same way as pharmaceutical drugs. Therefore, each new therapy must go through a rigorous process including pre-clinical animal trials, phased clinical studies, and pre-market review by the FDA prior to offering the treatment in the clinic.
And with stringent regulatory requirements comes prohibitive costs. Research animals, Phase I-III clinical trials, and the regulatory demands for good manufacturing practice (GMP) labs result in an extraordinarily costly process that may hinder the progress of new therapies. The cost of developing a new drug has even been estimated to reach billions of dollars.
Nevertheless, a complete lack of regulation of stem cell therapies – as is seen in many of the stem cell clinics springing up worldwide – is clearly problematic. Alarmingly, many clinics advertise claims related to medical diseases for which there is no scientific consensus that supports their safety or efficacy. Premature commercialization of unproven therapies not only puts patients at risk, but also jeopardizes the credibility of still-developing stem cell products.
One of the most exciting outlooks for stem cell therapy is the prospect of using one’s own stem cells for personalized medicine. Should the development of an autologous stem cell product really be regulated the same way as a pharmaceutical drug, which is aimed at treating huge populations of people? If not, how should stem cell products be regulated?
In an effort to make the transition of novel stem cell products to the clinic more seamless, some countries have made significant changes in regulations. For instance, in 2014, Japan broke out a separate regulatory system for stem cell products that softened legislation dramatically to require only limited safety and efficacy data. Some argue that countries with softer regulations and less stringent safety and efficacy milestones, such as Japan, have poised themselves to become the likely pioneers in the field of regenerative medicine.
Regulatory frameworks for the clinical application of stem cell products are still evolving in most countries, including the U.S. In March, the Reliable and Effective Growth for Regenerative health Options that improve Wellness (REGROW) Act was introduced to congress. This change in legislation would remove some of the regulatory hurdles that hinder the progress of biologic therapies.
Regardless, the FDA needs to establish a more reasonable regulatory system that can evaluate the safety and efficacy of stem cell products in a more efficient manner.
1. Berger, I., et al., Global Distribution of Businesses Marketing Stem Cell-Based Interventions. Cell Stem Cell, 2016. 19(2): p. 158-62.
2. Turner, L. and P. Knoepfler, Selling Stem Cells in the USA: Assessing the Direct-to-Consumer Industry. Cell Stem Cell, 2016. 19(2): p. 154-7.
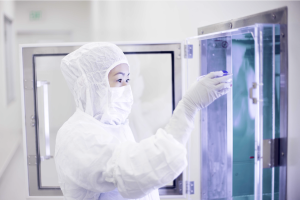
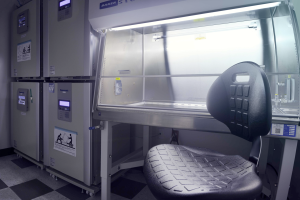
Generation of Human Stem Cells under Good Manufacturing Practice: Facility Update
Last year Allele dedicated a new building space for cleanroom operations to provide a cell banking service for personalized medicine. This facility will be the center of current Good Manufacturing Practice (cGMP) production of human induced pluripotent stem cells (iPSCs) using Allele’s proprietary synthetic mRNA platform. Over the past three months, progress to get the facility up and running has been substantial. Our facility includes four main modules: the reception area and doctors’ offices, a Fibroblast Isolation and Maintenance room, a Reprogramming and iPSC Maintenance room, and a Quality Control room. Air handling, which is a major component of the environmental control system, has been installed and validated. Equipment such as biosafety cabinets, incubators, and refrigerators have been installed and qualified, as well as equipment for performing essential quality control steps. To standardize personnel-related steps of cGMP processing, we have prepared rigorous SOPs and have extensively trained individual manufacturing operators. Overall, we are enthusiastic about the facility’s progress and are committed to delivering the best possible service as the industry leader in iPSC banking.
……………………………………………………………………………………………………………………
cGMP Compliance: What Does It Mean for Your Cell Lines?
As the promise for cell-based therapy grows, the interest in making clinically relevant cell lines has skyrocketed for industrial and academic researchers alike. For translation into human therapies, cell-based products must be made following current Good Manufacturing Practice (cGMP). Many groups have already claimed to generate cell lines that are “cGMP-compliant,” “cGMP-ready,” or “certifiable under cGMP.” But what does it take to be truly cGMP-compliant, and what practices can you introduce in your lab to comply with cGMP standards?
A common misconception in the United States is that a facility is granted a ‘cGMP license’ from the government to manufacture cGMP-grade products. Rather, the Food and Drug Administration (FDA) evaluates the manufacturing process for each product to determine if it is compliant with cGMP standards. The primary concern when it comes to deriving cell-based products for therapies is making sure that the product is derived in a safe and reproducible manner. To ensure maximum quality assurance, researchers should
• choose reliable, xenogeneic-free raw materials,
• establish and monitor a clean environment,
• qualify all equipment and software,
• remove variation in laboratory procedures by creating detailed Standard Operating Procedures (SOPs) and by providing rigid process validation at each step.
Nevertheless, even establishing robust quality assurance does not imply that the process is scalable for commercial production. In the world of biologics, “the product is the process.” A requisite step to ensure a smooth transition to cGMP practice is to ensure that the process of manufacturing is not altered due to changes in production scale. For example, depending on the therapy, millions or billions of cells may be required for a single patient. Therefore, it is in the best interest of the researchers to develop a scalable method at the beginning to avoid revamping the entire process (e.g., changing from adherent cells to suspension). Along these lines, the quality control (QC) requirements of cell-based products should be carefully considered and not have to include difficult-to-assay tests. For example, some cell lines have been qualified as cGMP-compliant upon conversion from research-grade conditions to cGMP quality standards. Rigorous tests were performed on the converted lines to ensure that the cells were free of contamination. Even though strict measures were carried out to ensure cGMP compliancy, deriving cell lines in this manner makes scalability and reproducibility a challenge. Ideally, the entire process of deriving cell products for clinical use should be performed under cGMP conditions: from the acquisition of human tissue to the manufacturing, testing, and storage of derivative cell products.
Another important consideration when instituting cGMP-compliance is documentation. Each process must be described with rigorous SOPs, the training of individual manufacturing operators must be well-documented, and the entire established process must be validated and well noted. Failure to document—in the eyes of the FDA—is often equated with failure to perform the underlying activity. It is equally important to remain ‘current.’ The FDA expects manufacturing processes to stay up-to-date with current regulations, even as policies change.
For an academic lab, closely aligning with cGMP standards can ensure that the resulting cell lines are comparable to other truly cGMP-produced products used during clinical trials. It is in the best interest of academic researchers to establish rigorous SOPs and use qualified reagents and equipment, even if it is not possible to carry out all steps in a certified cleanroom. Whenever possible, it is advisable to acquire truly cGMP cell lines from appropriate sources for preclinical projects; if prohibited by costs or other reasons, it is recommended to use a protocol that is as close to cGMP as possible.
Allele Biotechnology & Pharmaceuticals Forming Cell Banking Business for Personalized Medicine
Allele to Generate Human iPS Cells under Good Manufacturing Practice for Private Individuals for Potential Therapeutic Use and Future diagnostics; Cell Banking Scientific Advisory Board formed
October 06, 2015 11:25 AM Eastern Daylight Time
SAN DIEGO–(BUSINESS WIRE)–Allele Biotechnology & Pharmaceuticals, Inc. (“Allele”), a leader in the development of specialized cells for regenerative medicine and pharmaceutical drug discovery, today announced plans to form a commercial business for the banking of human induced pluripotent stem cells (iPSCs) by private individuals.
Allele is pleased to have Drs. Mahendra Rao and Joseph Paulauskis as the first members of its Scientific Advisory Board (SAB) for iPSC banking and cGMP production. Dr. Rao is a world-renowned scientist in the fields of stem cells and medicine, having served as the VP of Regenerative Medicine at Invitrogen, founding Director of the NIH Center for Regenerative Medicine, Chair of the Biological Response Modifiers Committee (BRMAC, now CTAGT) of the FDA, and he is currently Chief Strategy Officer at Q Therapeutics. Dr. Paulauskis is the Chief Operating Officer of Paradigm Dx as well as the Vice-President of Research and Biobanking for the International Genomics Consortium, and has previously held senior positions in pharmacogenomics at Pfizer. Allele plans to make additional appointments to the SAB as individuals with world-class experience and expertise are identified.
Human iPSCs are cells that can be grown to virtually infinite numbers and can become any cell in the human body, features which hold great promise for therapies that can alleviate or cure human disease. Allele’s business model recognizes that an individual can have their own cells ready for future therapeutic use via the generation and storage of iPSCs from that individual’s skin cells. While this is similar to what is done with newborn cord blood, iPSCs can be generated from humans of any age. The banking of human iPSCs for potential future therapeutic use is a relatively new industry with unprecedented potential, and Allele is benefitting from expert opinions internally and from current and future SAB members, ensuring a solid scientific and ethical foundation for this business.
In addition to serving its customers, Allele’s iPSC bank will be an unparalleled resource for biomedical research. Proper consent and privacy guardianship will allow thousands of iPSC lines with accompanying sequence database and health information to be made available from the bank to scientists and clinicians. Currently, iPSC banks are funded by government agencies at multi-million dollar costs per project; Allele’s model does not rely on tax dollars and provides potentially a larger bank of iPSCs of higher quality to aid research and treatment efforts. To this end, NIH Director Dr. Francis Collins recently announced the implementation of the Precision Medicine Initiative (PMI), the goal of which is for health care professionals to have the resources to take into account individual differences in genes, environments, and lifestyles that contribute to disease when providing treatments in the new era.
“We are happy to have the guidance from world leading experts in stem cells, biobanking, and cell therapy fields such as Drs. Rao and Paulauskis”, said Jiwu Wang Ph.D., President and CEO of Allele. “We believe that setting the bar high will be ultimately beneficial to future customers, fellow researchers, industry partners, and regulatory agencies alike. We are happy to see the recent release by the International Society for Stem Cell Research of a draft of ‘Guidelines for the Clinical Translation of Stem Cells’, whose principals we plan to follow closely. We also intend to obtain certification by the cord blood banking association AABB, if possible, and abide by other regulatory rules as they become public, such as the “Stem Cell Clinical Research Management (tentative)” by the Health Commission of China, if and when we move to operate under that jurisdiction”.
Towards the establishment of this business effort, Allele has recently purchased an 18,000 square-foot facility, located near its headquarters in San Diego, California. This new facility will be the center of cGMP-production of human iPSCs using Allele’s proprietary synthetic mRNA platform, a technology that generates cells with neither the random integration of foreign DNA nor the use of viruses or virus-based elements, drawbacks common to other technologies for making hiPSCs; thus, the “footprint-free” cells generated by Allele’s synthetic mRNA platform are optimally suited for therapeutic use, and Allele’s technology has been licensed for clinical trials by companies such as Ocata Therapeutics (formerly ACT). This effort received strong support from Yuan Capital and Yifang Ventures.
About Allele Biotechnology & Pharmaceuticals, Inc.
Allele Biotechnology and Pharmaceuticals, Inc. is a private, San Diego-based company that explores the mechanisms of biological processes to develop technologies and products for biomedical researchers. Allele utilizes proprietary non-integrating cellular reprogramming methods to generate human and non-human primate iPS cells, GMP-grade human iPS cells and their derivatives, and differentiated cell types. With additional expertise in genome modification and cell-based sensors/reporters, Allele provides advanced cell-based assays for drug discovery. Allele also has developed a wide variety of reagents including superior fluorescent proteins and camelid antibodies. The company has also been a leader in the RNAi field with its patents in Pol III promoter-driven siRNA, shRNA, and miRNA.
Contacts
Allele Biotechnology & Pharmaceuticals, Inc.
Matthew A. Singer, Ph. D.
Director of Business Development and Strategic Alliances
+1 858-587-6645, ext. 1
mattsinger@allelebiotech.com
www.allelebiotech.com
Categories
- Allele Mail Bag
- cGMP
- Customer Feedback
- Fluorescent proteins
- iPSCs and other stem cells
- nAb: Camelid Antibodies, Nanobodies, VHH
- Next Generation Sequencing (NextGen Seq)
- NIH Budget and You
- oligos and cloning
- Open Forum
- RNAi patent landscape
- SBIR and Business issues
- State of Research
- Synthetic biology
- Uncategorized
- Viruses and cells
- You have the power
Archives
- October 2018
- April 2018
- March 2018
- January 2018
- October 2017
- September 2017
- August 2017
- March 2017
- February 2017
- January 2017
- November 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- February 2016
- October 2015
- September 2015
- August 2015
- June 2015
- March 2015
- January 2015
- December 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- May 2012
- April 2012
- February 2012
- January 2012
- December 2011
- November 2011
- October 2011
- September 2011
- August 2011
- July 2011
- June 2011
- May 2011
- April 2011
- March 2011
- February 2011
- January 2011
- December 2010
- November 2010
- October 2010
- September 2010
- August 2010
- July 2010
- June 2010
- May 2010
- April 2010
- March 2010
- February 2010
- January 2010
- December 2009
- November 2009
- October 2009
- September 2009
- August 2009
- July 2009
- June 2009
- May 2009
- April 2009
- March 2009
- February 2009
- January 2009
- December 2008
- October 2008
- August 2008
- July 2008